Diagnosis
During the physical exam, your doctor will check your lymph nodes for swelling and use a stethoscope to listen to the sounds your lungs make when you breathe.
The most commonly used diagnostic tool for tuberculosis is a skin test, though blood tests are becoming more commonplace. A small amount of a substance called tuberculin is injected just below the skin on the inside of your forearm. You should feel only a slight needle prick.
Within 48 to 72 hours, a health care professional will check your arm for swelling at the injection site. A hard, raised red bump means you’re likely to have TB infection. The size of the bump determines whether the test results are significant.
Results can be wrong
The TB skin test isn’t perfect. Sometimes, it suggests that people have TB when they don’t. It can also indicate that people don’t have TB when they do.
You can have a false-positive result if you’ve been vaccinated recently with the bacille Calmette-Guerin (BCG) vaccine. This tuberculosis vaccine is seldom used in the United States but is widely used in countries with high TB infection rates.
False-negative results also can occur.
Blood tests
Blood tests can confirm or rule out latent or active tuberculosis. These tests measure your immune system’s reaction to TB bacteria.
These tests require only one office visit. A blood test might be useful if you’re at high risk of TB infection but have a negative response to the skin test, or if you’ve recently received the BCG vaccine.
Imaging tests
If you’ve had a positive skin test, your doctor is likely to order a chest X-ray or a CT scan. This might show white spots in your lungs where your immune system has walled off TB bacteria, or it might reveal changes in your lungs caused by active tuberculosis.
Sputum tests
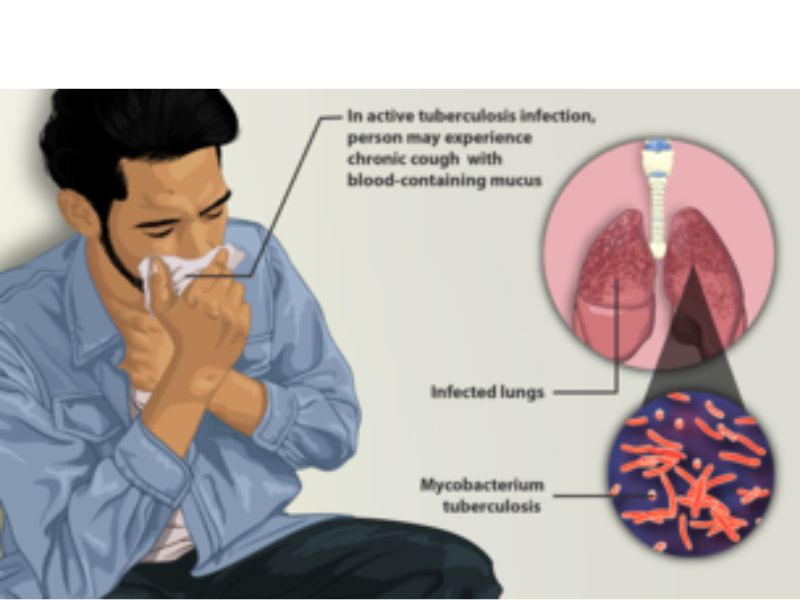
If your chest X-ray shows signs of tuberculosis, your doctor might take samples of your sputum — the mucus that comes up when you cough. The samples are tested for TB bacteria.
Sputum samples can also be used to test for drug-resistant strains of TB. This helps your doctor choose the medications that are most likely to work. Getting results of these tests can take four to eight weeks.
Treatment
If you have latent TB, your doctor might recommend treatment with medication if you’re at high risk of developing active TB. For active tuberculosis, you must take antibiotics for at least six to nine months.
The exact drugs and length of treatment depend on your age, overall health, possible drug resistance and where the infection is in your body.
Most common TB drugs
If you have latent tuberculosis, you might need to take only one or two types of TB drugs. Active tuberculosis, particularly if it’s a drug-resistant strain, will require several drugs at once. The most common medications used to treat tuberculosis include:
Isoniazid
Rifampin (Rifadin, Rimactane)
Ethambutol (Myambutol)
Pyrazinamide
If you have drug-resistant TB, a combination of antibiotics called fluoroquinolones and injectable medications, such as amikacin or capreomycin (Capastat), are generally used for 20 to 30 months. Some types of TB are developing resistance to these medications as well.
Some drugs might be added to therapy to counter drug resistance, including:
Bedaquiline (Sirturo)
Linezolid (Zyvox)
Medication side effects
Serious side effects of TB drugs aren’t common but can be dangerous when they do occur. All tuberculosis medications can be toxic to your liver. When taking these medications, call your doctor immediately if you have any of the following:
Nausea or vomiting
Loss of appetite
A yellow color to your skin (jaundice)
Dark urine
Easy bruising or bleeding
Blurred vision
Completing treatment is essential
After a few weeks, you won’t be contagious and you might start to feel better. Don’t stop taking your TB drugs — you must finish the full course of therapy and take the medications exactly as prescribed by your doctor.
Stopping treatment too soon or skipping doses can allow the bacteria that are still alive to become resistant to those drugs, leading to TB that is much more dangerous and difficult to treat.
A program called directly observed therapy (DOT) can help people stick to their treatment regimen. A health care worker gives you your medication so that you don’t have to remember to take it on your own.
Source: www.mayoclinic.org