In a spate of 42 days (24th May – 7th July 2023), the NHIA has paid its credentialed healthcare providers over GHC471 Million Cedis to cover claims submitted for periods up to January 2023. For the first time in several years, the NHIS is back into the accepted 90-day arrears window which means that health providers are only owed two (2) months of claims for February and March 2023.
Mandate
Ghana’s National Health Insurance Scheme (NHIS) is one of the major social intervention policies bequeathed to the nation by the Act of Parliament 650 (Act 650, 2003) as amended in 2012 with Act 852 to provide access to healthcare.
The NHIS Benefit Package covers over 95% of disease conditions that afflict residents of Ghana and has been detailed in the NHIS Act, Membership Handbook, and published on the website – www.nhis.gov.gh with services such as outpatient, in-patient, surgeries, oral, dental. There are over 550 formulations on the NHIS Medicines list to take care of all the diseases covered under the Scheme.
Membership & Health Providers
As of the end of 2022, the NHIS Scheme had an active membership of 17.2 million, representing approximately 55 percent of the population which is the highest since the inception of the Scheme.
The National Health Insurance Authority (NHIA) has credentialed over 4,500 health facilities across the country comprising Public, Private, Quasi, and Faith-based facilities with a variety of levels as CHPS Compounds, Health Centres, Pharmacies, Diagnostic Centres, Primary Hospitals, Secondary and Tertiary with the very latest being the International Maritime Hospital (GH) LTD (IMaH) in Tema Community One.
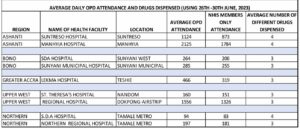
The public’s reliance on the use of the NHIS membership card to seek healthcare is still very encouraging across the country. A random sampling conducted to ascertain the use of the NHIS card in some regions of Ghana revealed the outcomes in the diagram above.
It is evident that on average over 80% of attendees to most public healthcare centers attend with their NHIS membership cards with at least three different drugs dispensed per visit. This cannot be said of a Scheme that is failing and accused of only dispensing paracetamol despite the rise in claims payments.
NHIA’s robust innovations
Over the past twenty (20) years, the NHIA has undertaken several reforms to make the NHIS more efficient, attractive, and sustainable ranging from the introduction of the instant issuance of a Biometric membership card system to the renewal of membership and self-enrolment using USSD (*929#) and applications (MyNHISApp) on mobile phones.
Especially since 2022, the NHIA has introduced robust innovations geared towards enhancing productivity, improving efficiency, and increasing visibility and brand recognition among others.
Some of the homegrown innovations comprise NHIS and Ghana Cards linkage, Partnership with premier league clubs to increase membership, the formation of National Committees against Illegal payments, the launch of the MyNHIS App, the Free Elderly Healthcare policy, and the Sunshine Policy.
NHIS and Ghana Cards linkage
Championing the national agenda of ‘One nation, one card for accessing healthcare services’ the NHIA in partnership with the National Identification Authority (NIA) intensified campaigns making it possible for people to use the Ghana card to access healthcare services effective May 01, 2021.
Partnership with local premier league Clubs
The Authority entered into a strategic partnership with four local premier league clubs to register team players, management staff together with their dependents, and some fans onto the NHIS. This first-of-a-kind created some awareness, excitement, and vibrancy for the brand during match days.
NHIS Benefit Package Expansion
With the aim of increasing the survival rate of children suffering from childhood cancers, the NHIS Benefit Package was expanded and made provision for the four main childhood cancers which are Neuroblastoma (childhood cancer of the jaw and abdomen), Leukemia (childhood cancer of the blood), Retinoblastoma (childhood cancer of the eye) and Wilms Tumor (childhood cancer of the kidney). Family Planning services were also added to the Benefit Package, after a successful pilot of the project in some selected districts nationwide in July 2022.
NHIS Reviews Tariffs Upwards
On July 1, 2022, the NHIS tariffs paid to health providers were adjusted upwards by 30% after consultation with critical stakeholders in the health sector. Within a space of seven months, the NHIA again in February 2023 increased upwardly its tariffs for medicines and services covered by the Scheme by a whopping 50% for medicines in the framework contracting plus an additional 30% marginal increase. Non-framework medicines were reviewed upwards by 20% while service tariffs across board have increased by 10%.
These adjustments were necessitated to correspond to the increasing prices of most active pharmaceutical ingredients and Management’s desire to minimize the incidents of illegal charges made of NHIS members by healthcare facilities. A recent study conducted by the NHIA revealed that since the adjustments, OPD bills to the Scheme have gone up by over 300 percent.
National Committees Set Up to Curb Illegal Payments
Copayments refer to the direct out-of-pocket payments for healthcare services and medications covered under the NHIS Benefit Package, and that adversely affect affordability and equality in accessing healthcare.
In an attempt to eliminate these financial barriers confronting the NHIS, Management set up decentralized Co-payment Committees at the Head Office, Regional and District offices with mandates that include engaging with the NHIA’s credentialed healthcare service providers and NHIS members who are sometimes compelled to pay such extra monies for services covered by the Scheme.
This is to strengthen the NHIA’s mandate of providing financial risk protection and improved access to healthcare for its members. The NHIA Board is currently reviewing the first national report submitted and will provide guidance on the appropriate sanctions to apply to facilities that will be found culpable. This age-old phenomenon has weakened some confidence in the Scheme and must stop.
Launch of MyNHIS App
Ending the year 2022, a digital platform known as ‘MyNHIS’ was unveiled in Tamale by the Vice President, Alhaji Dr. Mahamudu Bawumia.
The convenient mobile App solution empowers corporate clients and other citizens to use their Ghana cards to sign up for the NHIS without necessarily visiting any of the Scheme’s district offices for the same service.
The new App also enables NHIS members to securely pay registration and membership renewal fees from their mobile money wallets, and bank debit cards. The Mobile Application App issues a digitized NHIS card and provides a mechanism for the NHIA to fulfill its statutory obligations.
Most importantly, the innovation delivers a vastly improved renewal experience to NHIS members as it saves time and money, thereby making the Scheme much more accessible to all residents in Ghana and beyond.
Free Elderly Healthcare
Backed by the Ministry of Health, the NHIA Governing Board introduced the ‘Free Elderly Care Policy’ in December 2022. The policy guarantees a waiver of the mandatory 30-day waiting period and an exemption from the payment of premium and processing fees for all members aged 70 years and above.
President Nana Addo Dankwa Akufo-Addo approved the instant healthcare policy, embedded in the NHIS to address the many underlying health-related challenges faced by the older population in Ghana. This development gave greater priority to covering the healthcare needs of vulnerable groups in Ghana, especially those within the age bracket of 70 and above.
NHIA Claims Reimbursements
Over the years, previous management teams have had to traverse the difficult path of pooling funds from the Ministry of Finance (MOF) to pay for claims.
Though OPD cases and membership in the Scheme have seen some upward trends coupled with the tariff adjustments, the NHIA today pays on average between GHC150 – GHC200 Million per month as claims reimbursements.
The table below illustrates the total claims paid to providers between 2017 and 2022 as well as payments made as of 7th July of 2023.
| CLAIMS PAYMENT TO SERVICE PROVIDERS | |
| Year | Amount (GHS’million) |
| 2018 | 1,050.48 |
| 2019 | 803.43 |
| 2020 | 1,320.29 |
| 2021 | 1,115.28 |
| 2022 | 1,014.14 |
| *2023 | 1, 076.00 |
NB: 2023 payment is up to 7th July 2023.
Between May & June 2023 alone the NHIA paid over GHC 367 Million Cedis to over 4,000 health facilities across Ghana with a further payment of GHC104.5 Million paid on the 7th of July 2023.
The NHIA’s engagement with the MOF has improved significantly resulting in more frequent releases to the fund. Despite the general economic climate, the MOF has ensured that funds earmarked to support the NHIS are adequately protected and released on time.
Sunshine Policy
The ‘Sunshine Policy’ was launched as a platform to deepen accountability, transparency, and social auditing as the NHIS marks its 20th Anniversary. Since its launch in March 2023, suppliers of drugs to healthcare facilities and other stakeholders are able to log onto the NHIS website with privileged access to view payments made to deserving facilities.
Hitherto, the process was opaque which fuelled some stakeholders to wrongly accuse the NHIA of withholding payments due to facilities. This highest level of transparency has won the admiration of healthcare managers as a critical innovation.
Electronic Claims Management
With the intention to improve the claims management cycle by eliminating manual submission, vetting, and payment by the end of 2023, the NHIA is increasingly using the electronic Claims review system, crucial for addressing fraud and abuse to ensure the financial sustainability of the NHIS.
Throughout the first quarter of 2023, Four Thousand Five Hundred & Forty-Six (4,546) healthcare providers submitted claims at a total volume of 6,492,610 to the four Claims Processing Centres (CPC’s). Out of the total volumes of claims submitted, 86.3% were electronic whilst 13.7% were manual.
Barely two years ago, the reverse was perverse making the Scheme susceptible to fraud and abuse. This high-level efficiency being injected into the management of claims will reduce abuse resulting from human and manual interventions.
Furthermore, the NHIA is on the course soon to introduce the electronic verification of members at the point of seeking healthcare. This will further reduce the incidence where duplicate claims could be submitted or re-cycled thereby eliminating waste and fraud from the system.
Universal Health Coverage (UHC) Feasible
As the National Health Insurance Scheme (NHIS) continues to possibly impact people’s health-seeking behavior and contribute to better life expectancy outcomes for Ghanaians, the NHIA is committed to building a more resilient health insurance scheme that responds to the needs of all by providing more access to quality and affordable healthcare services.
By Karim Naatogmah









